Apple cider vinegar (ACV) is praised for various health benefits, but did you know it can also interact negatively with certain medications?
Potential Benefits:
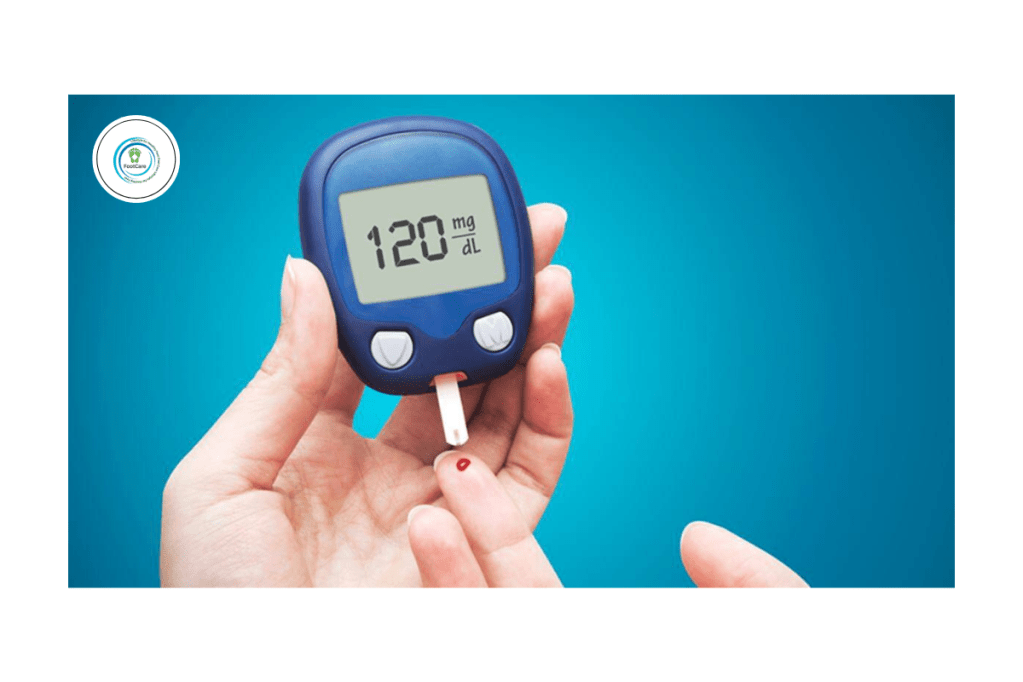
- 🌱 Helps manage blood sugar levels.
- 🥗 May support weight loss by boosting satiety.
- ❤️ Could improve cholesterol and heart health.
- 🍋 Contains antioxidants beneficial for overall health.
- 🌿 Skin Health: Has antibacterial and anti-fungal properties beneficial for various skin conditions.
👣 Benefits for Foot Care:
- 🦶 Reduces Foot Odor: Neutralizes bacteria responsible for unpleasant smells.
- 🍄 Treats Mild Foot Fungus: Combats fungal infections such as athlete’s foot and mild toenail fungus.
- 💦 Soothes Dry Skin: Can soften calluses and dry skin when used regularly.
- 🌊 Natural Exfoliant: Promotes removal of dead skin cells, leaving feet soft and smooth.
- 🛡️ Prevents Foot Infections: Antibacterial properties help reduce the risk of infections.
However, be cautious if you’re taking:
- 💊 Diabetes medications or insulin – ACV may significantly lower blood sugar, risking hypoglycemia.
- 💊 Diuretics (water pills): May further lower potassium levels, leading to electrolyte imbalance.
- 💊 Digoxin or heart medications: Could potentially affect potassium levels and cause irregular heart rhythms.
⚠️ Contraindications & Precautions:
- 🚫 Digestive Issues: Can irritate digestive system if consumed undiluted or in excess.
- 🦷 Dental Health: May damage tooth enamel due to acidity; always dilute and rinse mouth afterward.
- 💊 Medication Interactions: Can interact with medications for diabetes, heart conditions, and diuretics.
- 🤰 Pregnancy & Breastfeeding: Consult your healthcare provider before regular consumption.
🍎 Tips for Safe Consumption & Foot Use:
- 💧 Dilute 1–2 tablespoons ACV in a glass of water for drinking.
- 🛁 Foot Soak Recipe: Mix ½ cup ACV with warm water; soak feet for 15–20 mins, 1–2 times weekly.
- 🧽 After soaking, thoroughly dry feet to prevent fungal growth.
Always discuss with your healthcare provider before adding apple cider vinegar regularly, especially if you’re on medication or have chronic health conditions.
Your health matters! Have questions? Feel free to ask below. 🍎✨
Leave a comment